Abstract
During SARS-CoV-2 infection, a severe hypercoagulability state is observed due to the stimulus of multiple mechanisms of hemostasis, such as intrinsic and extrinsic coagulation pathways, activation of platelets, endothelial cells, monocytes and neutrophils endothelial and impaired fibrinolysis. As a consequence, thrombotic complications are common in the course of COVID-19. Microvesicles (MVs) are intracellular transmitters that participate in pathological conditions, such as inflammatory and infectious processes, and are capable of triggering prothrombotic mechanisms. Since MVs release is potentially associated with COVID-19-induced coagulopathy, our aim was to identify the moment during the time course of the disease when the stimulus for MVs release occurs and whether this was associated with adverse outcomes.
Therefore, we evaluate changes in MVs markers levels during the first month of SARS-CoV-2 infection in patients with severe disease (patients hospitalized in an intensive care unit - ICU) as compared to outpatients. We also evaluated the association between MVs markers and: acute phase inflammatory biomarkers (C-reactive protein, CRP), hypercoagulability (D-dimer) and death.
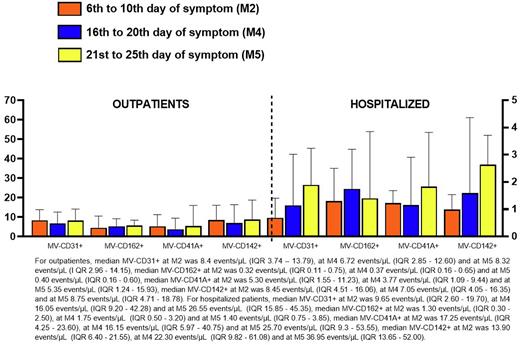
Blood samples of patients were collected on three occasions: before the 10th day of symptoms (6th to 10th day), in the third week of symptoms (16th to 20th) and in the fourth week of symptoms (21st to 25th day) for the quantification of the following MVs markers by flow cytometry: CD41A (platelet activation), CD162 (PSGL-1; leukocyte-platelet interaction), CD31 (endothelium-platelet interaction) and CD142 (tissue factor). Statistical tests of ANOVA with repeated measures, Mann-Whitney and regression methods were used.
The population studied was 85 patients, 65 outpatients and 20 ICU patients. Forty-three were men (51%), with a median age of 41 years old. The concentration of MVs expressing CD31+, CD41+, CD162+ and CD142+ were persistently elevated in patients who required ICU compared to outpatients at the 3 moments studied, except for the levels of MVs-CD31+ and MVs-CD142+ that were similar between ICU and outpatients in the fourth week of symptoms. However, despite the differences between the groups, there were no significant changes in the concentration of MVs during the course of the disease within the groups.
In subgroup analysis, we observed that increases in the levels of MVs-CD162+ and MVs-CD142+ in the third week of symptoms were associated with the risk of death (P=0.02 and P=0.06, respectively).
We also observed that before the 10th day of symptoms there was no correlation between MVs markers, CRP and D dimer levels. However, throughout the course of the disease the association between MVs, coagulability and inflammation was evident. In the third week of symptoms, D-dimer levels were correlated with MV-CD31+ (r=0.52; P<0.0001), MV-CD162+ (r=0.35, P=0.001), MV-CD41A+ (r=0.44, P<0.0001) and MV-CD142+ (r=0.47, P<0.0001). In the fourth week of symptoms, these correlations remained unchanged. CRP values from the third week of symptoms were correlated with MV-CD31+ (r=0.56, P=<0.0001), MV-CD162+ (r=0.48, P<0.0001), MV-CD41A+ (r= 0.41, P=0.0001), and MV-CD142+ (r=0.56, P<0.0001). In the fourth week of symptoms, these correlations remained unchanged.
In conclusion, MVs that express antigens related to platelet activation, leukocyte-platelet interaction and endothelium-platelet interaction, as well as those related to tissue factor are released during the course of COVID-19 in patients with severe disease. After the 4th week of symptoms, the release of these MVs was associated with signs of inflammation and hypercoagulability. Additionally, MVs that express tissue factor and leukocyte-platelet interaction antigens were particularly high among non-survivors, suggesting that these MVs may serve as markers of the risk of death. Finally, these findings suggest the participation of innate immunity and tissue factor pathways in the prognosis of COVID-19, and point towards a possible role of MVs as biomarkers of disease prognosis.
Disclosures
Villaça:Takeda: Consultancy, Honoraria; Bayer: Consultancy; Novo Nordisk: Consultancy; Sanofi: Consultancy, Honoraria; BioMarin: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.